Psoriasis, a chronic skin condition marked by the rapid accumulation of skin cells, results in thick, red, scaly patches. This autoimmune disorder involves the immune system mistakenly attacking healthy skin cells, leading to inflammation and excessive cell production. While not contagious, psoriasis can cause itching, discomfort, and joint pain, significantly affecting an individual’s quality of life.
Causes of Psoriasis
Several factors contribute to psoriasis development:
- Genetic Predisposition: Family history increases the risk, with certain genetic variations linked to susceptibility.
- Immune System Dysfunction: T cells, part of the immune response, mistakenly target healthy skin cells.
- Environmental Triggers: Infections, stress, skin injuries, smoking, and specific medications can trigger or worsen symptoms.
- Lifestyle and Diet: Obesity and excessive alcohol consumption may exacerbate symptoms, and dietary changes can impact individuals differently.
- Inflammatory Cytokines: Elevated levels of immune system proteins, like TNF-alpha and interleukins, are associated with psoriasis.
- Skin Microbiome: Disruptions in the skin’s microbiome may play a role in psoriasis development.
Symptoms of Psoriasis
Psoriasis manifests in various ways:
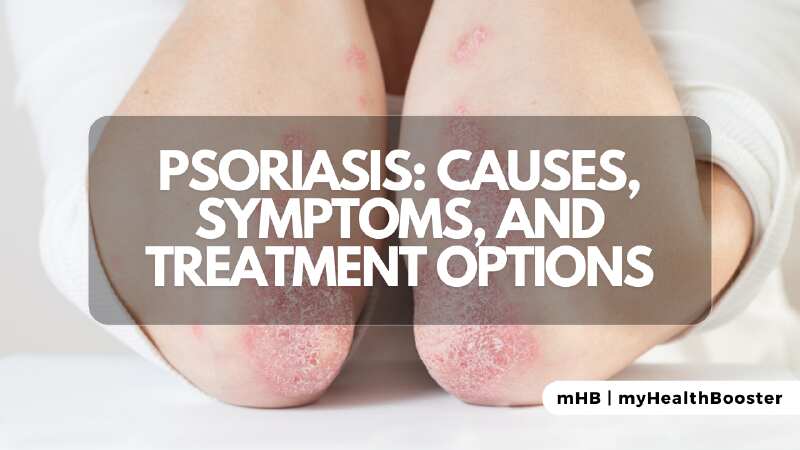
- Red, Raised Patches: Common in plaque psoriasis, appearing on elbows, knees, scalp, and lower back.
- Itching and Discomfort: Emotional distress often accompanies itching, burning, or soreness.
- Nail Changes: Psoriasis can affect nails, causing pitting, thickening, discoloration, or separation.
- Joint Pain: Psoriatic arthritis can lead to joint pain, swelling, and stiffness.
- Variations in Severity: Ranging from mild patches to severe coverage of the body, with remission and flare-ups.
Treatment of Psoriasis
Tailored treatment plans address individual needs and severity:
- Topical Treatments: Corticosteroids, vitamin D analogues, coal tar, or calcineurin inhibitors reduce inflammation and slow skin cell growth.
- Phototherapy: UV light exposure, natural or artificial, slows cell growth and reduces inflammation.
- Systemic Medications: Oral or injectable medications like biologics, methotrexate, and cyclosporine suppress immune overactivity.
- Lifestyle Changes: Stress management, weight control, and avoiding smoking and excessive alcohol improve symptoms.
- Biologic and Targeted Therapies: In severe cases, these therapies relieve immune responses.
Summary
While psoriasis is chronic, understanding its causes, recognizing symptoms, and exploring treatments enable effective management. Collaborating with healthcare providers to create personalized plans ensures individuals can lead fulfilling lives despite this skin condition.
FAQs
Q. What causes psoriasis?
A. The exact cause involves genetic, immune, and environmental factors.
Q. What are the common symptoms of psoriasis?
A. Symptoms include red, inflamed skin, itching, burning sensations, and dry, cracked skin that may bleed, affecting any part of the body.
Q. How is psoriasis diagnosed?
A. Dermatologists typically diagnose through a physical examination, sometimes performing a skin biopsy.
Q. What are the treatment options for psoriasis?
A. Options include topical creams, phototherapy, oral medications, biologics, and lifestyle changes, chosen based on type and severity.
Q. Can lifestyle changes help manage psoriasis?
A. Yes, maintaining a healthy diet, managing stress, avoiding triggers like smoking and excessive alcohol, and good skincare contribute to symptom management.